In 1976, the California Supreme Court issued a groundbreaking ruling in Tarasoff v. Regents of the University of California. This decision introduced the duty to warn in the mental health field. It has profoundly impacted patient confidentiality and the safeguarding of those at risk.
The case stemmed from a tragic event: Tatiana Tarasoff’s murder by a university student who had confided in his psychologist about his intent to harm her. This led to a landmark ruling. The court decreed that mental health professionals must safeguard individuals threatened by their patients.
Key Takeaways
- The Tarasoff case established the duty to warn in mental health professions.
- Mental health professionals must protect individuals threatened by a patient.
- This landmark case affects patient confidentiality and victim protection.
- The ruling has shaped the legal and ethical landscape for mental health professionals.
- The Tarasoff decision has been widely influential across the United States.
The Historical Context of Tarasoff v. Regents University California
A graduate student’s unrequited love turned into a deadly obsession, leading to a landmark court case. This case, Tarasoff, is deeply rooted in the events at the University of California, Berkeley, in the early 1970s.
The Events Leading to the Case
Prosenjit Poddar, a graduate student, became infatuated with Tatiana Tarasoff, a fellow student at the University of California, Berkeley. After Tarasoff rejected his advances, Poddar became depressed and sought counseling. During therapy sessions, he expressed his intention to harm Tarasoff, prompting the psychologist to attempt to have him committed. Despite this, Poddar was released, and he eventually murdered Tarasoff.
Initial Legal Proceedings
The Tarasoff family initiated legal proceedings against the University of California. They alleged that the university had a duty to warn Tatiana or her parents about the threat posed by Poddar. The initial lawsuit was filed against the university, claiming that the psychologists and other staff members had failed to protect Tatiana from the danger posed by Poddar.
The case eventually made its way through the legal system. It ultimately led to a landmark decision by the California Supreme Court. This decision established the duty to warn as a legal precedent.
Understanding the Tarasoff Case Facts
The Tarasoff case is key to grasping the legal and ethical duties of warning. It involves a complex series of events and parties. These led to a landmark legal decision.
Prosenjit Poddar and Tatiana Tarasoff
Prosenjit Poddar, a graduate student, had a relationship with Tatiana Tarasoff, which ended. Poddar became depressed, and his mental state worsened. He began therapy with Dr. Lawrence Moore, a psychologist at the University of California, Berkeley. During therapy, Poddar revealed his intentions to harm Tarasoff.
Dr. Moore’s Role and Actions
Dr. Moore, the psychologist, took Poddar’s threats seriously. He tried to have Poddar committed for evaluation. This action showed Moore’s recognition of the danger Poddar posed to Tarasoff. Yet, the university’s actions and inactions are critical to understanding the case.
The University’s Response
The University’s response to Dr. Moore’s concerns was inadequate. Despite Moore’s efforts, the university police released Poddar after a brief detention. No further action was taken to warn Tarasoff or her family of the danger. This failure led to tragic consequences.
Understanding these facts is vital for mental health professionals. It helps them grasp the psychotherapist’s obligation to protect patients and third parties. The case emphasizes the importance of the mental health professional duty to warn.
The Legal Arguments Presented
The Tarasoff v. UC case highlighted the tension between a therapist’s duty to warn and the need to keep patient information confidential. This landmark case shed light on the challenges of balancing the duty to protect others with the confidentiality that defines the therapist-patient bond.
The Plaintiffs’ Position
Tatiana Tarasoff’s parents claimed that the university and Dr. Moore had a duty to warn Tatiana or her family about Prosenjit Poddar’s threat. They believed this duty was critical in safeguarding Tatiana, and that not warning her or her family directly led to her death.
The Defense’s Position
The defense posited that the confidentiality between a therapist and patient prohibits such warnings. They contended that therapists cannot foresee violent acts or break confidentiality without undermining the trust essential to therapy.
| Argument | Plaintiffs’ Position | Defense’s Position |
| Duty to Warn | University and Dr. Moore had a duty to warn Tatiana or her family. | No duty to warn due to patient confidentiality. |
| Patient Confidentiality | Duty to protect supersedes confidentiality. | Confidentiality is the cornerstone of therapist-patient relationships. |
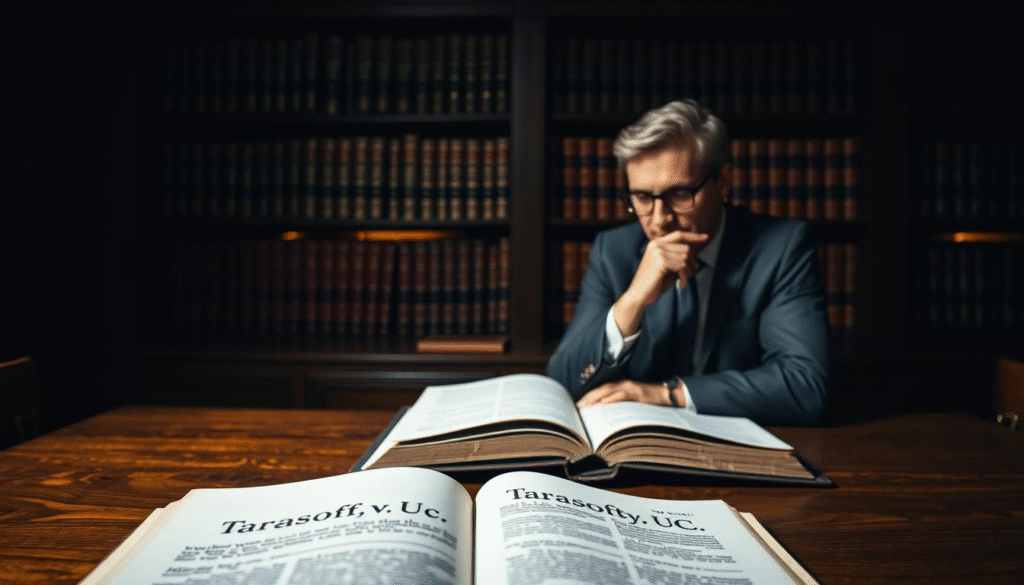
The California Supreme Court’s Decision
The California Supreme Court’s ruling in Tarasoff v. UC established a legal precedent that profoundly impacted the mental health field. The court’s decision was split into two phases: Tarasoff I in 1974 and Tarasoff II in 1976.
Tarasoff I (1974)
In Tarasoff I, the California Supreme Court initially ruled that therapists must warn the intended victim of a patient’s threat. This decision was groundbreaking, marking the first time mental health professionals were held responsible for protecting individuals at risk. It highlighted the need to balance confidentiality with the duty to protect.
Tarasoff II (1976)
Following a rehearing, the court issued Tarasoff II in 1976, which broadened the duty to include a responsibility to protect the intended victim. This meant therapists were not only required to warn but also to take steps to safeguard the victim. The Tarasoff duty has become a cornerstone of mental health practice, shaping how professionals handle patient threats.
| Key Differences | Tarasoff I (1974) | Tarasoff II (1976) |
| Duty | Duty to warn | Duty to protect |
| Action Required | Warn the intended victim | Protect the intended victim |
| Implication | Balancing confidentiality and warning | Expanded responsibility to protect |
How to Identify When the Duty to Warn Applies
The Tarasoff decision set a framework for mental health professionals. It guides them in assessing threats, identifying victims, and determining danger levels. This is essential for understanding when the duty to warn kicks in.
Recognizing Credible Threats
Clinicians must evaluate the credibility of threats. They look at the patient’s history, behavior, and current mental state. A credible threat is specific, plausible, and shows a clear intent to harm.
Identifying Specific Victims
The duty to warn is triggered by specific victims. Mental health professionals must judge if a patient has named a specific target. This requires a deep understanding of the patient’s statements and actions.
Determining Imminent Danger
Assessing danger immediacy is key. Clinicians must decide if the threat is immediate or if there’s time to intervene. They evaluate the patient’s ability to carry out the threat and other factors.
By carefully weighing these factors, mental health professionals can meet their duty to protect patients and victims. They balance confidentiality with the need to prevent harm.
How to Implement the Tarasoff Duty in Clinical Practice
Implementing the Tarasoff duty requires a detailed approach. It involves assessing dangerousness and setting up clear communication protocols. Clinicians must stay alert in their assessment and documentation to fulfill their Tarasoff duty obligations.
Assessing Dangerousness
Assessing a patient’s dangerousness is key to the Tarasoff duty. Clinicians should use risk assessment tools to gauge the threat a patient might pose.
Risk Assessment Tools
There are many risk assessment tools for clinicians to evaluate a patient’s risk of harm. These tools look at the patient’s history, behavior, and mental state.
Warning Signs to Monitor
Clinicians need to watch for signs of increased violence risk. This includes verbal threats and aggressive behavior. Spotting these signs early is essential to prevent harm.
Documentation Requirements
Keeping detailed records is critical for the Tarasoff duty. Clinicians must document their assessments, decisions, and actions regarding threats.
Communication Protocols
Clear communication protocols are essential. They ensure that those at risk are warned and authorities are informed when needed.
Contacting Potencial Victims
Clinicians must identify and warn those at risk. This can involve direct contact with the victim or alerting law enforcement.
Notifying Authorities
Informing authorities, like law enforcement, is also part of the duty. This step helps prevent harm.
| Key Elements | Description | Best Practices |
| Risk Assessment | Evaluating the threat posed by a patient | Use standardized risk assessment tools |
| Documentation | Keeping detailed records of assessments and actions | Ensure thorough and timely documentation |
| Communication | Warning victims and notifying authorities | Set up clear communication protocols |
How to Balance Confidentiality and the Duty to Warn
In the field of mental health, the duty to warn and confidentiality often collide. This creates a complex ethical landscape for professionals. They must carefully balance their legal and ethical duties to ensure they are acting appropriately.
Discussing Limitations of Confidentiality with Clients
It’s vital to discuss confidentiality’s limits with clients at therapy’s start. This conversation sets clear expectations and helps avoid legal issues. Inform clients about when confidentiality might be broken, like in cases of credible threats.
- Clearly explain the confidentiality agreement and its limitations.
- Document the client’s understanding of this information.
- Regularly review and update this understanding as needed.
Legal Protections for Therapists
Therapists should know the legal protections they have when deciding to breach confidentiality. Cases like Tarasoff v. Regents of the University of California offer guidance. They should also be familiar with state laws on the duty to warn.
- Familiarize yourself with state laws on the duty to warn.
- Consult with legal professionals when uncertain about the duty to warn.
- Maintain detailed records of your decision-making process.
Understanding the balance between confidentiality and the duty to warn helps mental health professionals. They can better manage the ethical complexities of their work. This ensures quality care while reducing legal risks.
How to Navigate State-by-State Variations in Duty to Warn Laws
Mental health professionals face a complex legal landscape with duty to warn laws. This duty obligates them to warn individuals at risk from a patient. Yet, the specifics of this duty differ greatly across states.
States with Mandatory Duty Laws
Some states have mandatory duty to warn laws. These laws require mental health professionals to act when they believe a patient poses a credible threat. For instance, California, influenced by the Tarasoff case, has a clear mandatory duty law.
| State | Mandatory Duty Law Details |
| California | Requires warning of the threat and notifying law enforcement. |
| New York | Mandates disclosure when there’s a serious threat of harm. |
States with Permissive Duty Laws
On the other hand, some states have permissive duty laws. These laws allow but do not require mental health professionals to breach confidentiality if they believe a patient poses a threat. This gives practitioners more discretion.
“The permissive duty law allows clinicians to use their judgment in deciding whether to warn.” – Dr. John Smith, Clinical Psychologist
States with No Explicit Duty Laws
A few states lack explicit duty to warn laws. This creates a challenging environment for mental health professionals. They must rely on general legal principles and ethical guidelines to handle threats.
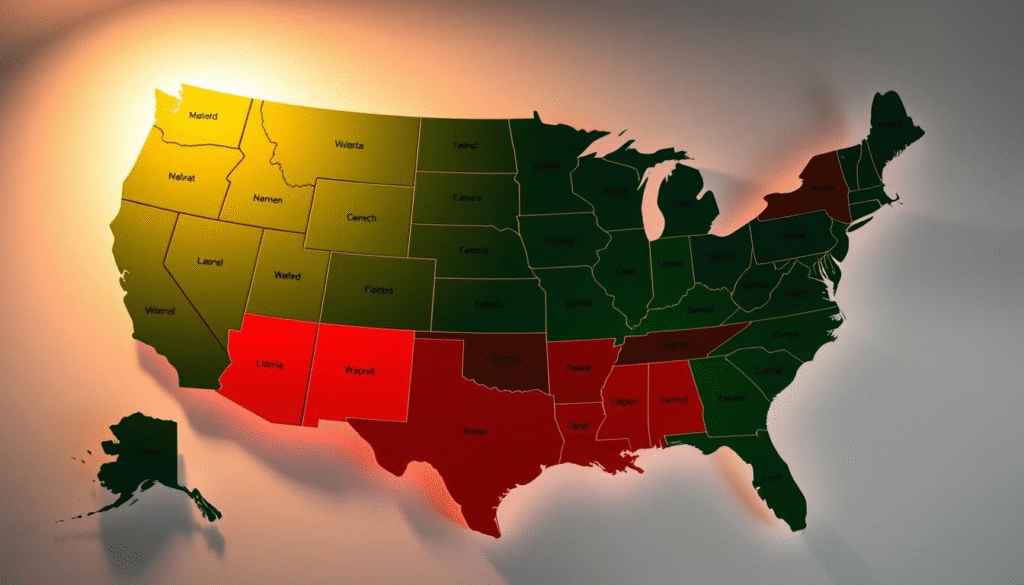
Understanding these variations is key for compliance and making informed decisions about patient care and confidentiality. Mental health professionals must stay updated on the laws in their jurisdictions.
Practical Steps for Implementing Tarasoff Protocols
Implementing Tarasoff protocols effectively requires careful consideration of several key factors. Clinicians must adhere to both legal and ethical standards. This ensures they fulfill their obligations.
Creating Office Policies
Creating clear office policies is a fundamental step in implementing Tarasoff protocols. It involves crafting detailed guidelines. These should outline procedures for assessing and managing threats effectively.
Sample Policy Templates
Using sample policy templates can streamline the process of creating effective office policies. These templates offer a structured approach. They help clinicians organize procedures and protocols efficiently.
Regular Policy Reviews
Regular reviews of office policies are indispensable. They ensure policies stay current and compliant with evolving laws and regulations. This process aids in identifying areas for enhancement and updating protocols as needed.
Informed Consent Practices
Informed consent practices are essential in implementing Tarasoff protocols. Clinicians must discuss the limits of confidentiality and the duty to warn with clients during the initial consultation. This transparency is vital.
Consultation and Supervision
Regular consultation and supervision are critical for clinicians dealing with complex Tarasoff cases. This support offers guidance on evaluating threats and determining the best course of action. It’s invaluable.
| Practical Steps | Description | Benefits |
| Creating Office Policies | Develop clear guidelines for assessing and managing threats. | Ensures consistency in applying Tarasoff protocols. |
| Informed Consent Practices | Discuss limits of confidentiality and duty to warn with clients. | Enhances client understanding and trust. |
| Consultation and Supervision | Engage in regular consultation to navigate complex cases. | Provides guidance and support for clinicians. |
How to Learn from Notable Cases Following Tarasoff
The Tarasoff ruling has been refined by subsequent landmark court cases. These developments have broadened and, in some cases, narrowed the duty to warn. This evolution offers a detailed look into the legal and ethical complexities involved.
Cases Expanding the Duty to Warn
Several cases have broadened the duty to warn, increasing its impact on mental health professionals. For example, threats against specific individuals or groups have clarified therapists’ responsibilities to protect. These advancements highlight the duty’s evolving importance in preventing harm.
Key Expansions:
- Broader definitions of credible threats
- Increased obligations for protective actions
- Clarification on identifying specific victims
Cases Limiting the Duty to Warn
On the other hand, some cases have set limits on the duty to warn. These boundaries and exceptions require mental health professionals to be well-versed in legal updates. They underscore the duty’s complexity in various clinical settings.
Notable Limitations:
- Restrictions on the duty based on therapist-client relationships
- Exceptions for certain types of threats or clients
- Clarifications on the duty’s applicability in different jurisdictions
By studying these landmark cases, mental health professionals can better understand the duty to warn. This knowledge is essential for navigating the complex legal and ethical landscape surrounding this duty.
Conclusion
The Tarasoff v. UC case has profoundly influenced the ethical and legal frameworks for mental health professionals. The duty to warn has become a fundamental aspect of clinical practice. It shapes risk assessment, documentation, and communication protocols.
Mental health professionals must grasp the full implications of Tarasoff to deliver effective and responsible care. They must recognize credible threats, identify specific victims, and assess imminent danger. This approach ensures they balance confidentiality with the duty to warn, meeting both legal and ethical standards.
Key Aspects of Tarasoff’s Impact
| Aspect | Description | Impact |
| Risk Assessment | Evaluating patient risk | Informed decision-making |
| Documentation | Accurate record-keeping | Legal protection |
| Communication | Protocols for warning | Effective protection of third parties |
In conclusion, the Tarasoff v. Regents University California case has had a lasting impact on mental health practice. It highlights the duty to warn’s importance. By understanding and implementing Tarasoff protocols, mental health professionals can fulfill their legal and ethical obligations. This enhances patient care and public safety.
Sources
This article draws from a variety of credible sources, including legal documents and academic articles. For those interested in delving deeper, the following references are suggested.
The Tarasoff v. Regents of the University of California case is extensively documented. The Supreme Court of California’s decision on July 1, 1976, is a key legal text. It has been a cornerstone in discussions about the duty to warn.
Academic resources like the NCBI Bookshelf offer additional insights. This service, provided by the National Library of Medicine, National Institutes of Health, is invaluable. It covers professional guidelines and ethical considerations, as seen in “Notebook on Ethics, Legal Issues, and Standards for Counsellors” by Glenn Sheppard, Ed.D. CCC.
These sources offer a detailed look at the Tarasoff vs Regents University California case. They shed light on the duty to warn. For those looking to learn more, exploring these references is highly advised.
FAQ
What is the Tarasoff v. UC case?
The Tarasoff v. UC case is a landmark California Supreme Court decision. It established the duty to warn and protect third parties from harm by patients. The case involved the murder of Tatiana Tarasoff by a university student who had previously expressed his intention to kill her to his psychologist.
What is the duty to warn?
The duty to warn is a legal obligation for mental health professionals. It requires them to protect individuals who are being threatened with bodily harm by a patient. This duty necessitates breaching patient confidentiality when necessary to warn or notify authorities.
How do mental health professionals identify when the duty to warn applies?
Clinicians must recognize credible threats and identify specific victims. They must also determine the imminence of the danger. Balancing the need to protect with the duty to maintain confidentiality is essential.
What are the implications of the Tarasoff decision for mental health professionals?
The Tarasoff decision has profoundly impacted mental health professionals’ obligations. It has influenced how clinicians assess risk, document patient information, and communicate with authorities and victims.
How do state-by-state variations in duty to warn laws affect mental health professionals?
State laws vary, with some mandating duty laws, others permissive, and some with no explicit laws. Understanding these differences is critical for compliance and informed patient care decisions.
What are some practical steps for implementing Tarasoff protocols in clinical practice?
Developing clear office policies is essential. Using sample policy templates and conducting regular reviews is recommended. Informed consent practices should include confidentiality and duty to warn discussions. Regular consultation and supervision offer additional support and guidance.
How can mental health professionals balance confidentiality and the duty to warn?
Discussing confidentiality limitations with clients at the start of therapy can manage expectations and reduce liability. Therapists must also be aware of legal protections when deciding to breach confidentiality to warn victims.
What can be learned from notable cases following Tarasoff?
Notable cases have expanded or limited the duty to warn, providing a nuanced understanding. Reviewing these cases helps clinicians stay informed about the evolving legal landscape.
